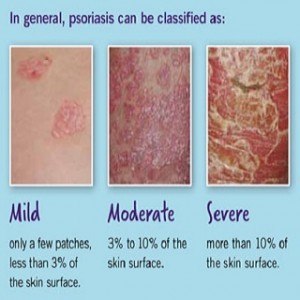
 Psoriasis is a chronic genetic autoimmune disorder that causes skin cells to grow too quickly. As a result, patches of skin will appear thick, white, silvery, or red and tend to bleed and crack. Usually, skin cells grow slowly and flake off about every 4 weeks. New skin cells grow to replace the outer layers of the skin as they shed. But with psoriasis, new skin cells move rapidly to the surface of the skin in days instead of weeks.
Psoriasis is a chronic genetic autoimmune disorder that causes skin cells to grow too quickly. As a result, patches of skin will appear thick, white, silvery, or red and tend to bleed and crack. Usually, skin cells grow slowly and flake off about every 4 weeks. New skin cells grow to replace the outer layers of the skin as they shed. But with psoriasis, new skin cells move rapidly to the surface of the skin in days instead of weeks.
The cells build up and form thick patches called plaques. The patches range in size from small to large. They most often appear on the knees, elbows, scalp, hands, feet, or lower back.
Seven and a half million Americans are affected by psoriasis. It is most common in adults, but children and teens can get it too.
What causes psoriasis?
The cause of psoriasis isn’t fully known, but it’s thought to be related to an immune system problem with cells in your body. More specifically, one key cell is a type of white blood cell called a T lymphocyte or T cell. Normally, T cells travel throughout the body to detect and fight off foreign substances, such as viruses or bacteria. If you have psoriasis, however, the T cells attack healthy skin cells by mistake, as if to heal a wound or to fight an infection.
Overactive T cells trigger other immune responses. The effects include dilation of blood vessels in the skin around the plaques and an increase in other white blood cells that can enter the outer layer of skin. These changes result in an increased production of both healthy skin cells and more T cells and other white blood cells. This causes an ongoing cycle in which new skin cells move to the outermost layer of skin too quickly — in days rather than weeks. Dead skin and white blood cells can’t slough off quickly enough and build up in thick, scaly patches on the skin’s surface. This usually doesn’t stop unless treatment interrupts the cycle.
Just what causes T cells to malfunction in people with psoriasis isn’t entirely clear. Researchers have found genes that are linked to the development of psoriasis, but environmental factors also play a role.
Symptoms of Psoriasis
- Plaques of red skin, often covered with loose, silver scales. This is the symptom most commonly associated with psoriasis Such lesions can be extensive, itchy and painful. Cracking and bleeding may occur. In the most severe cases, these patches merge with one another to cover entire surface areas of the body.
- Irritated patches of skin. Skin patches and dots are raised and thick, ranging from pink-red salmon to red in color. Often times these skin patches or skin dots are, like noted in the aforementioned, covered in silvery scales.
- Redness on elbows, knees, trunk and scalp. Though these are the main places in which psoriasis symptoms are seen, symptoms can occur anywhere on the body.
- Change and disfiguration of nails. Thickening, yellow-brown spots, dents and pits in the nail surface, separation of nail from base and crumbling of the actual nail may occur.
- Severe dandruff. Plaques of silver scales or crust may develop as loose flakes constantly shed.
Treatment for Psoriasis
- Topical medications. Topical options include steroids, vitamin D analogues, topical retinoids, and coal tar.
- Oral medications. Oral drugs used to treat severe or stubborn psoriasis include retinoids, cyclosporine, methotrexate, hydroxyurea, and other immunomodulators.
- Light therapy. Natural and artificial light, including ultraviolet light, can be used to treat psoriasis. The most recent therapies developed use ultraviolet B, which is effective without having to take medications that increase sensitivity to sunlight.
- Dietary changes
- Exercise
- Supplements